ELECTRODIAGNOSTIC FEATURES OF TRUE NEUROGENIC THORACIC OUTLET SYNDROME
ELECTRODIAGNOSTIC FEATURES OF TRUE NEUROGENIC THORACIC OUTLET SYNDROME
ELECTRODIAGNOSTIC FEATURES OF TRUE NEUROGENIC THORACIC OUTLET SYNDROME
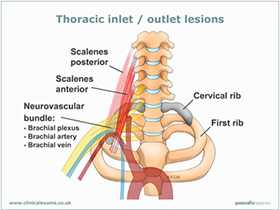
Thoracic outlet syndrome (TOS) is defined as a variety of disorders resulting from compression, injury, or irritation of the nerves and/or blood vessels in the lower neck and upper chest area.
Thoracic outlet syndrome is named for the space (the thoracic outlet) between your lower neck and upper chest where this grouping of nerves and blood vessels is found.
Causes for TOS include a cervical rib, old fracture of the clavicle, soft tissue abnormalities (scalenus muscle), tumors or large lymph nodes in the upper chest or underarm area, repetitive stress injuries and others.
The signs and symptoms of TOS include neck, shoulder, and arm pain, numbness or impaired circulation to the affected areas.
There are 3 major kinds of TOS: Neurogenic, Venus and Arterial.
True neurogenic thoracic outlet syndrome (TNTOS) is rare, with an estimated incidence of only 1 per 1,000,000.
In April 2014, Tsao et al reported on the electrodiagnostic features of a TNTOS. They reported the electrodiagnostic (EDX) features of 32 patients with surgically verified true neurogenic thoracic outlet syndrome (TN-TOS).
Methods included a retrospective record review. They found uniform EDX evidence of a chronic axon loss process that affected the lower portion of the brachial plexus and disproportionately involved the T1 more than the C8 sensory and motor fibers. Because of this relationship, the medial antebrachial cutaneous sensory nerve (T1) and median motor (T1>C8) study combination was abnormal in 89%, whereas response combinations that primarily assessed the C8 fibers were less frequently affected. The researchers concluded that characteristic EDX features of TN-TOS are T1>C8 nerve fiber involvement. A comprehensive EDX examination of the lower plexus with contralateral comparison studies is imperative to diagnose this disorder accurately.
In terms of clinical examination, special tests can be applied to rule out TOS:
Adson’s test: with the patient sat on the edge of the examining table, the practitioner abducts, extends and laterally rotates the patient’s symptomatic arm whilst monitoring the radial pulse and instructs the patient to rotate their head towards the elevated arm whilst holding their breath. A diminution in radial pulse and/or an aggravation in symptoms indicates a positive test. This test sensitive to thoracic outlet lesions result from an elongated C7 TP or a cervical rib. However, this test is notorious for yielding false positives.
Halstead test: with the patient sat on the edge of the examining table, the practitioner abducts, extends and laterally rotates the patient’s symptomatic arm whilst monitoring the radial pulse and instructs the patient to rotate their head away from the elevated arm whilst holding their breath. A positive is indicated by an aggravation in symptoms. This test is more sensitive to a thoracic outlet lesion due to a pathological process involving the anterior scalene muscle.
Costoclavicular manoeuvre: instruct the patient to sit on the edge of the examining table, with both shoulders retracted and depressed and the arms abducted to 30°. An aggravation in symptoms indicates a positive. This test is sensitive to clavicular involvement in thoracic outlet syndrome. A definitive diagnosis can be reached via arteriography and nerve conduction testing.
1. Tsao, B. E., Ferrante, M. A., Wilbourn, A. J. and Shields, R. W. (2014), Electrodiagnostic features of true neurogenic thoracic outlet syndrome. Muscle Nerve, 49: 724–727
2. Syrimis A: Clinical Examinations.